By Taylor Knopf
When a patient expresses a mental health concern to their primary care provider, that typically generates a referral to a behavioral health specialist. Then that specialist contacts the patient to schedule an appointment. It can take multiple tries to get the appointment scheduled, and then the first available slot is sometimes weeks away. By then, the opportune moment to engage with the patient has likely passed, or their mental health issue may have escalated into a crisis.
A UNC Health family medicine and pediatrics practice in east Pittsboro is eliminating those delays.
In October, the practice hired a mental health provider to collaborate with doctors in the clinic and meet with patients — that same day. If during an appointment a patient says they are struggling with depression or grief, the provider asks if they would like to meet the clinic’s licensed clinical social worker, Jacqueline Fuentes.
No phone calls, no delay.
“Then I go right into the exam room and get to work with them, in the moment,” Fuentes said. “There’s that window of opportunity to just engage and say, ‘Hey, this is who I am’ and then understand what their concerns are.”
Fuentes works with patients of all ages and often brings family members into the process — particularly caregivers of pediatric patients and older adults. The goal is for Fuentes to meet a patient the same day they say they’d like support. She then often schedules follow-up appointments for the same day or week.
This position is designed to support a patient in the short term — ideally for about eight sessions. Fuentes connects patients with other mental health resources for long-term counseling or other services. And she continues to check in with her patients throughout their relationship with the primary care practice.
“So I think that warm handoff is really special,” she said.
Since Fuentes started seeing patients through this new initiative in October, she’s had more than 70 warm handoff encounters like these, and she’s served 125 patients overall. This process keeps the patient at the center of the communication, she said, instead of there being a multi-step referral process across departments and providers, where the mental health and primary care providers rarely interact.
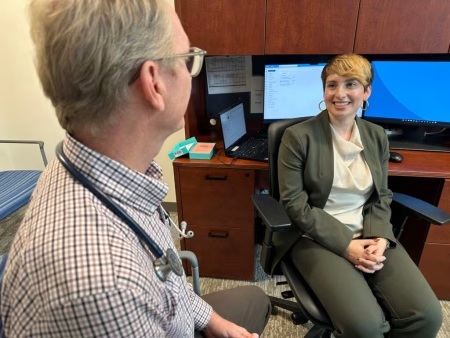
Erik Butler, a physician and medical director of the Pittsboro practice, said in a news release that this initiative has transformed care for his patients.
“The ability to recognize behavioral health needs and immediately connect patients with [Fuentes] has been next-level care,” he said. “In just six weeks, we’ve collaborated more than I have cumulatively with mental health specialists in my career.”
Not one-size-fits-all
Fuentes works with families of children with behavioral health needs, couples going through marital issues, patients navigating grief and loss, domestic violence situations and patients with substance use issues who receive medication for opioid use disorder from the clinic.
“It’s been a really unique way to … adapt to what people need, which I think is the best way to do behavioral health,” she said. “There’s not a one-size-fits-all.”
Some patients will always be uncomfortable with the idea of seeing a mental health provider, and they might never have engaged with services if they had not been embedded in the primary care practice. Other families at the Pittsboro practice have been seeing providers there for generations, so there’s a built-in trust. This could make them more open to meeting with Fuentes because she’s collaborating directly with their trusted family doctor.
“I’ve worked with some elderly patients, later in life stressors and caregiver support for that particular population, which I think has been really helpful,” Fuentes said. “I think that possibly a lot of these individuals have never interfaced with a behavioral health or a mental health provider, and so being embedded in primary care … it’s been this very easy handoff.”
A face-to-face introduction to a mental health provider also increases the likelihood of a patient following up with mental health services. A 2023 study published in the Journal of Adolescent Health looked at the difference in engagement between patients who were given a warm handoff to a mental health provider versus those who were electronically referred. Those with a warm handoff introduction were three times more likely to participate in their follow-up appointment.
Paying for a flexible model
The warm handoff model at the Pittsboro clinic is the first of its kind for UNC Health. It was built on years of work to bring mental health care into primary care settings so patients can get quicker access to care.
Clinic leaders also believe this kind of connection can reduce the need for more intensive crisis services later.
While Fuentes bills insurance for her sessions with patients, due to the flexible nature of her position, not all of her clinic time fits nicely into a billable code. Donor funding secured by UNC Health fills the gaps that insurance does not cover and makes it possible for patients at the Pittsboro clinic to get impromptu mental health support during their primary care visits.
UNC Health leaders say they hope to replicate this model across more primary care practices in the state and continue to seek funding opportunities to make that possible.
“Traditionally, great programs like this have been challenging to fund under current reimbursement structures, and we could not move forward without support to sustain the model,” Adam Goldstein, a physician and professor of family medicine at UNC who helped secure funding for this model, said in a news release. “Linking interested donors with embedded mental health resources struck a positive chord among community members.”











